<研究機器/温冷覚・温冷刺激> intercross-212


皮膚感覚の定量化と異常感覚の原因探査
- 医療機器をベースにした信頼性
- 豊富なソフトウェアで広がる拡張性
- 動物から人試験まで可能なプローブラインナップ
を基にして研究機器として再設定した製品です。
ソフトウェアのフレキシビリティおよび使用可能なプローブ種類の豊富さなど研究機器としての個性を有します。
intercross-212は、ペルチェ素子と熱流センサの組み合わせによる熱刺激および感覚閾値測定により
温覚・冷覚・温痛覚・冷痛覚などの多彩な皮膚感覚評価パラメータを検出します。
独自の方法である熱流方式は、制御および測定にも利用され、開始時温度を皮膚温度に合わせる役目や、閾値としての測定値としても活用可能です。
弊社の装置を利用した感覚の評価は多くの研究者から指示され米国CDCをはじめ国内海外で多くの論文が発表されております。
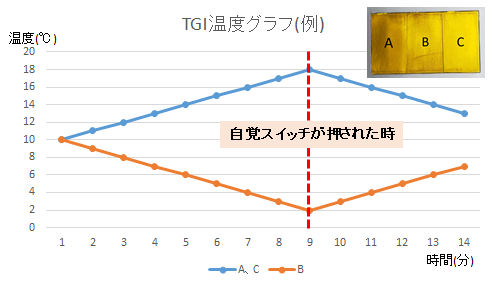
Thermal Grill Illusion
intercross-212は3つのペルチェ素子を個別にコントロールが可能
温刺激と冷刺激の同時刺激によりTGI(Thermal Grill Illusion)を実現
Offset Pain relief
intercross-212はプローブ温度を任意に設定可能であり、かつ被験者が操作する
VAS入力装置
刺激温度とVAS数値を同時して測定・保存可能
そのためoffsetと呼ばれるPain-Reliefが可能
製品本体:intercross-212
ディスプレイ一体型の本体は、持ち運び可能なサイズの装置です。
医療機器であるintercross-220をベースにしているため安全対策や温度制度の信頼性も高い設計です。
ソフトウェア:
・温冷覚閾値測定
・Pain Research
・痛覚刺激
・TGI
オプション
・昇降台(右側:使用例)


intercross-212論文
・FABILLAR Jr, Jaime, et al. “Research Presentations in Yogyakarta, Indonesia: Academic Conference Report.” Journal of Oral Health and Biosciences 38.1 (2025): 1-3.
intercross-210論文
・”Short-term collagen nerve wrapping facilitates motor and sensory recovery from nerve degeneration in a sciatic nerve injury rat model.” Sonohata, Motoki, et al. Journal of Pain Research (2023): 1683-1695.
・”Free gait in a shallow pool accelerates recovery after exercise in model mice with fibromyalgia.” Nakata, Taiki, et al. Journal of exercise rehabilitation 16.5 (2020): 398.
Doi, Atsushi, et al. “Whole body vibration accelerates the functional recovery of motor nerve components in sciatic nerve-crush injury model rats.” Journal of exercise rehabilitation 19.3 (2023): 149.
・”Time-dependent responses in brain activity to ongoing hot stimulation in burning mouth syndrome.” Kohashi, Ryutaro, et al. Journal of oral science 62.2 (2020): 170-174.
・”P-14 背部および腰部における温・冷刺激面積の違いによる温・冷感受性の差異に関する研究 (ポスターセッション I).”宮本. 人間-生活環境系シンポジウム報告集 38 (2014): 95-98.
・”P-16 温熱的中立~ 寒冷環境における温冷刺激を知覚する温度と不快を知覚する温度に関する研究: 青年男性被験者の頭部と末梢部の場合 (ポスターセッション II).”宮本.人間-生活環境系シンポジウム報告集 39 (2015): 139-142.
・”Contribution of skin hydration to warmth detection among individuals.” Sawai, Hiroko, and Tetsuo Kurahashi. 2020 IEEE 2nd Global Conference on Life Sciences and Technologies (LifeTech). IEEE, 2020.
・”Observations of cold-induced vasodilation in persons with spinal cord injuries.”
Fujita, Yasuhisa, et al. Spinal Cord 62.4 (2024): 170-177.
・”Paced breathing causes tonic change rather than phasic modulation of superficial venous diameter.”Matsumoto, Miharu, Nobuko Hashiguchi, and Hiromitsu Kobayashi. Journal of physiological anthropology 44.1 (2025): 13.
・”Differential cutaneous thermal sensitivity in humans: method of limit vs. method of sensation magnitude.”Seo, Yongsuk, and Jung-Hyun Kim. International Journal of Environmental Research and Public Health 18.23 (2021): 12576.
・”Regional differences in facial skin blood flow responses to thermal stimulation.”Miyaji, Akane, Shohei Hayashi, and Naoyuki Hayashi. European journal of applied physiology 119.5 (2019): 1195-1201.
・”Short-and long-term effects of using a facial massage roller on facial skin blood flow and vascular reactivity.”Miyaji, Akane, Kaori Sugimori, and Naoyuki Hayashi. Complementary therapies in medicine 41 (2018): 271-276.
・”Thermal sensation after the 10-km open-water swimming in cool water depends on the skin’s thermal sensitivity rather than core temperature.”Fujimoto, Tomomi, et al. International Journal of Sports Physiology and Performance 19.1 (2023): 28-33.
・”E6 (S)-5 Comparison of indices associated with skin conductance responses evaluating for emotional changes induced by tactile thermal stimuli.” Kotani, Kentaro, et al. The Japanese Journal of Ergonomics 53.Supplement1 (2017): S98-S101.
・”Association between anxiety and descending pain modulation of thermal stimuli in patients with burning mouth syndrome: a cross-sectional study.”Ozasa, Kana, et al. Journal of Oral & Facial Pain and Headache 36.1 (2022): 3050.
・”Effects of local cold and heat stimuli on cutaneous thermal sensitivity and inter-threshold zone at rest and during exercise.” Kim, Dae-Hwan, et al. Exercise Science 30.4 (2021): 453-461.
・”Observations of cold-induced vasodilation in persons with spinal cord injuries.” Kamijo, Yoshi-ichiro, et al. (2022).
・”Effects of low-intensity exercise on local skin and whole-body thermal sensation in hypothermic young males.” Fujimoto, Tomomi, et al. Physiology & Behavior 240 (2021): 113531.
・”Drop homotopic effects of masseter-muscle pain on somatosensory sensitivity in healthy participants.”Hayakawa, Hidetoshi, et al. Scientific Reports 11.1 (2021): 10575.
・”Effects of Autogenic Training on Pain Modulation in Burning Mouth Syndrome: A Preliminary Study.”Takizawa, Keita, et al. Cureus 17.3 (2025).
・”Effect of sustained jaw opening on fatigue, pressure pain sensations, and stiffness in the masticatory muscles.” Watanabe, Kosuke, et al. International Journal of Oral-Medical Sciences 21.4 (2023): 131-136.
・”Hypocapnia attenuates local skin thermal perception to innocuous warm and cool stimuli in normothermic resting humans.”Fujimoto, Tomomi, et al. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 324.1 (2023): R120-R127.
・”Warm‐, hot‐and pain‐related neural activities depending on baseline skin temperatures.”Nakata, Hiroki, R. Kakigi, and M. Shibasaki. European Journal of Pain 22.10 (2018): 1791-1799.
・“Body Regional Heat Pain Thresholds in Korean Young Males. Diss.“박성진.서울대학교 대학원, 2017.
・”Altered pain modulation to noxious heat thermal stimuli in burning mouth syndrome.” Nishihara, Chisa, et al. Oral Diseases 26.8 (2020): 1777-1782.
・”Exercise Does Not Prevent Thermoregulatory Adaptation to Cold Stress During the Winter Season.” Kim, Dae-Hwan, et al. Exercise Science 33.4 (2024): 468-476.
・”Analysis of mechanism of referred pain in orofacial region.”早川英利. (2022).
・”気流を知覚する風速と冷覚閾値の関係 25℃・50% 環境下における前腕部への曝露の場合.”宮本征一, and 桃井良尚.人間‐生活環境系シンポジウム報告集 第 45 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2021.
・”Impairment of pain inhibition in patients with burning mouth syndrome.”西原千紗. (2022).
・”Intersegmental differences in facial warmth sensitivity during rest, passive heat and exercise.”Kim, Jung-Hyun, et al. International Journal of Hyperthermia 36.1 (2019): 653-658.
・”Alteration of somatosensory profile in patients with burning mouth syndrome.”渡邉広輔. (2019).
・”Temporal modulation of brain responses during ongoing hot stimulation in burning mouth syndrome.”小橋龍太郎. (2019).
・”温度弁別能と温度感受性の身体部位差と加齢による変化.”深沢太香子, and 谷明日香. 繊維製品消費科学 58.1 (2017): 108-114.
・”日本人壮年期女性における下腿と足の温度感受性.”深沢太香子, and 倉橋萌菜. 人間‐生活環境系シンポジウム報告集 第 44 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2020.
・”Involvement of psychological factors and the menstrual status in burning mouth syndrome.”小笹佳奈. (2022).
・”局所温冷刺激による温冷覚閾値の測定方法の違いによる 温冷覚閾値の差異に関する
研究.”宮本征一, and 近藤恵美.人間‐生活環境系シンポジウム報告集 第 46 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2022.
・”各部位における冷刺激を知覚する温度および 不快を知覚する温度に関する研究.”
宮本征一, and 井口拓海. 人間‐生活環境系シンポジウム報告集 第 43 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2019.
・”Body regional heat pain thresholds using the method of limit and level: a comparative study.” Park, Sungjin, Sang-Hyun Roh, and Joo-Young Lee. European journal of applied physiology 119.3 (2019): 771-780.
・”関西と北海道における温冷覚の閾値および不快を知覚する温度の地域差に関する研究.”宮本征一.人間‐生活環境系シンポジウム報告集 第 47 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2023.
・”各部位における温刺激を知覚する温度および 不快を知覚する温度に関する研究.”井口拓海, and 宮本征一.人間‐生活環境系シンポジウム報告集 第 43 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2019.
・“Cutaneous Thermal Thresholds Induced by Conductive and Radiant Heat Stimulations. Diss.”Roh, Sang-Hyun. 서울대학교 대학원, 2024.
・”気流を知覚し始める風速の閾値に関する研究 その 1 異なる風温下での青年男性の前腕を対象とした場合.”大下颯真, et al. 人間‐生活環境系シンポジウム報告集 第 47 回人間-生活環境系シンポジウム報告集. 人間‐生活環境系学会, 2023.
・”機能性ウェアへの水分散布による蒸発性熱放散促進 および紫外線散乱による温熱的快適性向上.”芝﨑学, 久保博子, and 難波真理. デサントスポーツ科学 42 (2022): 3-23.
・”Empirical Study of Physiological Characteristics Accompanied by Tactile Thermal Perception: Relationship Between Changes in Thermal Gradients and Skin Conductance Responses.” Shinoda, Takafumi, et al. International Conference on Human Interface and the Management of Information. Cham: Springer International Publishing, 2016.
intercross-200論文
・”Measuring heat flux and amount of heat as indexes of cold pain threshold.” Shimo, Kazuhiro, Shigeyuki Suzuki, and Takahiro Ushida. Pain Research 27.1 (2012): 17-26.
・”Age-related differences in cutaneous warm sensation thresholds of human males in thermoneutral and cool environments.” Tochihara, Yutaka, et al. Journal of Thermal Biology 36.2 (2011): 105-111.
・”Effects of a Traditional Japanese Medicine Goshajinkigan, Tokishigyakukagoshuyushokyoto on the Warm and Cold Sense Threshold and Peripheral Blood Flow.” Hang, Liu, et al. Health 6 (2014): 757-763.
・”熱流束, 総熱量測定による痛覚評価の検討.” 下和弘, 鈴木重行, and 牛田享宏. PAIN RESEARCH 27.1 (2012): 17-26.
・”Accuracy and reliability of thermal threshold measurement in the chin using heat flux technique.” Kawano, Teppei, et al. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 108.4 (2009): 500-504.
・”Improvement in neuropathy outcomes with normalizing HbA1c in patients with type 2 diabetes.” Ishibashi, Fukashi, et al. Diabetes Care 42.1 (2019): 110-118.
・”The expanded bead size of corneal c‐nerve fibers visualized by corneal confocal microscopy is associated with slow conduction velocity of the peripheral nerves in patients with type 2 diabetes mellitus.” Ishibashi, Fukashi, et al. Journal of diabetes research 2016.1 (2016): 3653459.
・”Sex differences in age-related changes on peripheral warm and cold innocuous thermal sensitivity.” Inoue, Yoshimitsu, et al. Physiology & behavior 164 (2016): 86-92.
・”Sodium glucose cotransporter-2 inhibitor protects against diabetic neuropathy and nephropathy in modestly controlled type 2 diabetes: Follow-up study.” Ishibashi, Fukashi, Aiko Kosaka, and Mitra Tavakoli. Frontiers in Endocrinology 13 (2022): 864332.
・”Analysis of clinical usefulness of the heat flux technique: predictability of the recovery from neurosensory disturbances in the chin undergoing mandibular sagittal split ramus osteotomy.”
Satoh, Yuriko, et al. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 106.5 (2008): 637-643.
・”Correlation between sudomotor function, sweat gland duct size and corneal nerve fiber pathology in patients with type 2 diabetes mellitus.” Ishibashi, Fukashi, et al. Journal of diabetes investigation 5.5 (2014): 588-596.
・”Effects of a Traditional Japanese Medicine Goshajinkigan, Tokishigyakukagoshuyushokyoto on the warm and cold sense threshold and peripheral blood flow.” Tsukada, Rika, et al. Health 6.8 (2014): 757-763.
・”Analysis and comparison of clinical results of bilateral sagittal split ramus osteotomy performed with the use of monocortical locking plate fixation or bicortical screw fixation.”
Kabasawa, Yuhji, et al. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 116.5 (2013): e333-e341.
・”A new evaluation method for neurosensory disturbance in the chin of patients undergoing mandibular sagittal split ramus osteotomy: an application of the heat flux technique.” Kabasawa, Yuhji, et al. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 102.6 (2006): 719-724.
・”Impact of normoglycemia in reducing microvascular complications in patients with type 2 diabetes: a follow-up study.” Ishibashi, Fukashi, and Mitra Tavakoli. Frontiers in Endocrinology 9 (2018): 52.
・”Body regional influences of L-menthol application on the alleviation of heat strain while wearing firefighter’s protective clothing.” Lee, Joo-Young, et al. European journal of applied physiology 112.6 (2012): 2171-2183.
・”Cutaneous warm thresholds at rest and thermoregulatory responses during whole body warming: Comparisons between tropical and temperate indigenes.” Lee, Joo-Young, et al. Editors: James D Cotter, Samuel JE Lucas and Toby Mündel: 133.
・”Cutaneous thermal thresholds of tropical indigenes residing in Japan.” Lee, Joo-Young, et al. Journal of Thermal Biology 36.7 (2011): 461-468.
・”Cutaneous warm and cool sensation thresholds and the inter-threshold zone in Malaysian and Japanese males.”Lee, Joo-Young, et al. Journal of Thermal Biology 35.2 (2010): 70-76.
・”PERIPHERAL THERMAL THRESHOLDS AND THERMOEFFECTORS THRESHOLD ZONE IN MALAYSIAN AND JAPANESE MALES.”
Lee, Joo-Young, et al.
・”Lower thermal sensation in normothermic and mildly hyperthermic older adults.” Takeda, Ryosuke, et al. European journal of applied physiology 116.5 (2016): 975-984.
・”月経周期による女性の皮膚温度感受性の変化および空調環境への応用.”大塚優希, 山下穂南美, and 安河内朗.日本生理人類学会誌 21.4 (2016): 141-150.
・”The preferential impairment of pupil constriction stimulated by blue light in patients with type 2 diabetes without autonomic neuropathy.”Ishibashi, Fukashi, et al. Journal of diabetes research 2017.1 (2017): 6069730.
・”Intradermal administration of magnesium sulphate and magnesium chloride produces hypesthesia to mechanical but hyperalgesia to heat stimuli in humans.” Ushida, Takahiro, et al. Journal of neuroinflammation 6.1 (2009): 25.
・”The impact of glycemic control on retinal photoreceptor layers and retinal pigment epithelium in patients with type 2 diabetes without diabetic retinopathy: a follow-up study.” Ishibashi, Fukashi, Aiko Kosaka, and Mitra Tavakoli. Frontiers in Endocrinology 12 (2021): 614161.
・Hayashi, Kazuhiro, et al. “Effects of virtual reality‐based exercise imagery on pain in healthy individuals.” BioMed Research International 2019.1 (2019): 5021914.
Kim, Yung-Bin, et al. “Sensitivity to cutaneous warm stimuli varies greatly in the human head.” Journal of Thermal Biology 69 (2017): 132-138.
・”Thermal sensation during mild hyperthermia is modulated by acute postural change in humans.” Takeda, Ryosuke, et al. International journal of biometeorology 60.12 (2016): 1925-1932.
・“Body Regional Heat Pain Thresholds in Korean Young Males. Diss.” 박성진. 서울대학교 대학원, 2017.
・”若年者における口腔内粘膜・口唇・口唇周辺の温冷覚閾値測定の試み.”阿部雅子, 内田幸子, and 戸田貞子.日本官能評価学会誌 16.1 (2012): 43-50.
・”Sweat gland function in Thai and Japanese males in relation to physical training.”
Inoue, Yoshimitsu, et al. Proceedings of the 13th international conference of environmental ergonomics. 2009.
・”熱流束方式温冷覚閾値計を用いた痛覚閾値測定の試み.”下和弘, et al.理学療法学 Supplement Vol. 37 Suppl. No. 2 (第 45 回日本理学療法学術大会 抄録集). 日本理学療法士協会 (現 一般社団法人日本理学療法学会連合), 2010.
・”温度弁別能と温度感受性の身体部位差と加齢による変化.”深沢太香子, and 谷明日香. 繊維製品消費科学 58.1 (2017): 108-114.
. “熱流束および総熱量を指標とした冷覚および痛覚の定量的感覚検査の試み.”下和弘, and 鈴木重行理学療法学 Supplement Vol. 38 Suppl. No. 2 (第 46 回日本理学療法学術大会 抄録集). 日本理学療法士協会 (現 一般社団法人日本理学療法学会連合), 2011.
・”Thinning of macular neuroretinal layers contributes to sleep disorder in patients with type 2 diabetes without clinical evidences of neuropathy and retinopathy.”Ishibashi, Fukashi, and Mitra Tavakoli. Frontiers in endocrinology 11 (2020): 69.
・”Chang P Arai, Katsutoshi Suetomi and Makoto Nishihara.”Ushida, Takahiro, Osamu Iwatsuº, and Kazuhiro Shimo. journal of Neuroinflammation 6 (2009): 625.
・”加齢に伴う温度感覚の減弱は全身持久力の向上で改善できるか?.”岡崎和伸, et al. デサントスポーツ科学 38 (2017): 55-63.
“機能性ウェアへの水分散布による蒸発性熱放散促進 および紫外線散乱による温熱的快適性向上.”芝﨑学, 久保博子, and 難波真理.デサントスポーツ科学 42 (2022): 3-23.
“手足の ‘しびれ’と皮膚感覚感受性との関係―糖尿病性末梢神経障害のある患者を対象に―.”赤松公子, and 深井喜代子.日本看護技術学会誌 13.2 (2014): 160-171.
・”健常者の三叉神経領域の熱流束による温冷覚閾値.”田坂明子, et al. 日本口腔科学会雑誌 56.4 (2007): 367-373.














